You can tell your CPAP pressure is too high when you struggle to exhale, develop frequent mask leaks, experience bloating/aerophagia, dry mouth or nasal irritation, eye dryness from escaping airflow, or sudden AHI fluctuations. This happens because the excess airflow exceeds what your airway actually needs to stay open, leading to leaks and physical discomfort. Recognizing these signs early is critical because, according to research in the American Journal of Respiratory and Critical Care Medicine, discomfort from over-pressurization is a primary reason patients abandon therapy.
How do I know if my CPAP pressure is too high?
You will likely feel a distinct physical struggle against the incoming air, specifically when trying to breathe out. You might also wake up with a dry mouth, notice your mask making burping noises due to broken seals, or feel bloated in the stomach immediately after waking up.
Can high CPAP pressure cause aerophagia?
Yes, excessive pressure often forces air into the esophagus and stomach rather than just the lungs. According to a 2007 Chest Journal clinical analysis (Chest, 2007), aerophagia is a frequent symptom of pressure levels that exceed the patient's physiological requirement, causing bloating and gas.
Does high CPAP pressure make CPAP leaks worse?
Absolutely, as pressure that is too high for your mask rating or fit can break the silicone seal against your skin. This causes air to hiss out into your eyes or onto your cheeks, which compromises the effectiveness of the therapy.
Can high pressure interfere with sleep quality?
Yes, high pressure can fragment sleep by causing frequent awakenings to adjust the mask, swallow air, or clear a dry throat. A study in the journal Sleep (2006) found that patient discomfort from pressure intolerance is a leading cause of poor sleep quality and reduced adherence.
When should CPAP pressure be adjusted?
Only a sleep specialist should adjust CPAP pressure. Changing it yourself can lead to under-treatment, worsening AHI, or even the development of central apnea. While APAP machines adjust automatically, they do not replace the need for a proper clinical titration study.
Symptom and Solution Summary
|
Symptom |
Underlying Cause |
Clinical Meaning |
Corrective Action |
|
Hard to exhale |
Pressure > expiratory tolerance |
Exhalation resistance, breath stacking |
Increase EPR, use Ramp, consider APAP |
|
Mask leaks |
Seal displaced by airflow |
Pressure > mask capacity |
Switch to full face mask or adjust fit |
|
Aerophagia |
Air entering the stomach |
Pressure intolerance |
Reevaluate titration; consider BiPAP |
|
Dryness |
High airflow dehydrates the mucosa |
Mucosal irritation |
Add heated humidifier + heated tubing |
What Is CPAP Pressure & What Does “Too High” Mean?
CPAP pressure is simply the force of air, measured in centimeters of water (cmH2O), that is delivered to keep your upper airway open while you sleep. As defined by the NCBI Bookshelf page on Continuous Positive Airway Pressure, this therapy relies on delivering constant positive airway pressure to maintain airway patency throughout the night. However, CPAP pressure becomes "too high" when the delivered airflow exceeds the amount actually required to keep your airway stable. At this point, you may begin experiencing difficulty exhaling, increased mask leaks, or general discomfort, an interpretation supported by ResMed’s guidance on CPAP pressure effects.
CPAP Pressure
CPAP pressure is the continuous positive airway pressure (measured in cmH2O) that prevents upper airway collapse during sleep, as defined in the NCBI Bookshelf CPAP reference (Pinto et al., 2025).
High CPAP Pressure
High CPAP pressure is a setting that exceeds the minimum necessary for airway patency, potentially causing discomfort, leaks, or air swallowing, a phenomenon described in ResMed’s CPAP Pressure Settings guidance.
Pressure Intolerance
Pressure intolerance refers to an inability to tolerate airflow due to elevated pressure, impaired exhalation, or sensitivity to EPAP levels. This concept aligns with clinical explanations from Dental Sleep Medicine’s CPAP intolerance overview, which lists pressure-related discomfort as a major barrier to use.
Aerophagia
Aerophagia is the involuntary swallowing of air into the esophagus and stomach when CPAP pressure exceeds physiologic tolerance, leading to bloating or abdominal discomfort. This condition is clinically described by the Cleveland Clinic’s aerophagia resource.
AHI Instability
AHI instability refers to fluctuations in apnea-hypopnea index (AHI) values caused by mismatches in pressure, mask leaks, or pressure discomfort. This interpretation aligns with the ScienceDirect AHI topic overview, which explains how improper pressure can interfere with accurate scoring.
EPAP / IPAP
EPAP holds the airway open during exhalation, while IPAP supports airflow during inhalation. High EPAP commonly contributes to difficulty exhaling. This distinction is consistent with the respiratory mechanics outlined in the Comprehensive Physiology Study (Javaheri & Dempsey, 2013).

What Are the Signs Your CPAP Pressure Is Too High?
CPAP pressure is considered “too high” when the delivered airflow significantly exceeds what your airway physiologically requires to stay open, leading to specific and clinically recognized symptoms. As noted in the Merck Manual OSA overview (Strohl, 2022), this excess pressure often manifests as intolerance or physical discomfort that disrupts therapy. Furthermore, experts in UpToDate OSA management (Kryger & Malhotra, 2022) highlight that recognizing these signs early is crucial for long-term adherence and effective treatment.
Difficulty Exhaling
When the Expiratory Positive Airway Pressure (EPAP) is set too high, you may feel like you are breathing out against a heavy wall of air. This resistance can cause breath stacking or significant respiratory discomfort, a phenomenon explained by the physiologic mechanics of sleep apnea in the Comprehensive Physiology Study (Javaheri & Dempsey, 2013).
Aerophagia / Bloating
High CPAP pressure can force air past the esophageal sphincter and into your stomach instead of just your lungs. This leads to morning bloating and gas, a condition clinically linked to pressure intolerance in studies from the journal Sleep (Ayas et al., 2006).
Mask Leaks
Excessive airflow often destabilizes the mask cushion, lifting the seal away from your face and causing noisy leaks. Clinical findings in the Chest Journal (2007) confirm that leak-related intolerance significantly increases when pressure settings overpower the mask's capacity to maintain a seal.
Dry Mouth or Nasal Dryness
A strong, continuous stream of air can rapidly evaporate moisture from your mucosal surfaces, leaving your nose and throat parched. Research on humidification in the Chest Journal (Massie et al., 1999) indicates that this drying effect is exacerbated by high pressure, especially if humidification is not adjusted to match the airflow.
Eye Irritation From Upward Leaks
When pressure is too high, air frequently escapes through the top of the mask and blows directly into the orbital area. An analysis in the American Journal of Respiratory and Critical Care Medicine (2014) notes that this specific type of leak often results in morning eye dryness, redness, or conjunctival irritation.
High Residual AHI
Surprisingly, excessive pressure can distort airflow signals or create leak-driven artifacts that falsely inflate your Apnea Hypopnea Index (AHI). As detailed in the ScienceDirect AHI topic overview, accurate scoring relies on stable pressure, while a study in the Journal of Clinical Sleep Medicine (Yeom et al., 2021) showed that pressure-induced event misalignment can lead to misleading data.
Sleep Fragmentation
The physical struggle to exhale or the noise from leaks can cause frequent micro-arousals that prevent you from reaching deep sleep. Research in Sleep (Lankford, 2005) highlights how CPAP intolerance directly correlates with these fragmented sleep patterns and reduced therapy benefits.
Chest Discomfort
Some sensitive patients may experience chest tightness or respiratory muscle fatigue because their chest wall has to work harder against the incoming pressure. This side effect is evaluated in the Journal of Clinical Medicine (Farré, Gozal & Montserrat, 2021), which links incorrect pressure titration to increased musculoskeletal strain during sleep.
Key Signs Snapshot
-
Difficulty exhaling due to elevated EPAP
-
Mask leaks caused by excessive airflow pushing the seal
-
Aerophagia and morning bloating from swallowed air
-
Dry mouth or nasal passages from high airflow
-
Eye dryness or irritation from upward leaks
-
Elevated residual AHI caused by distorted airflow signals
-
Sleep fragmentation from intolerance-related arousals
-
Chest tightness or discomfort at high pressure settings
What Causes High CPAP Pressure?
CPAP pressure can become "too high" due to a variety of factors, ranging from physiologic changes in your body to airway resistance or even specific device behavior in Auto-CPAP (APAP) modes. High pressure generally occurs when the machine detects resistance, instability, or leaks that signal a need for more airflow to maintain airway patency. This mechanism is documented in adult OSA management guidelines from UpToDate (Kryger & Malhotra, 2022) and Merck Manual OSA physiology (Strohl, 2022).
Clinical Causes
Incorrect or Outdated Titration
An initial titration study provides a snapshot of your needs at that moment, but those settings may no longer match your current airway requirements. Over time, these outdated settings can lead to pressures that exceed what is necessary for effective therapy, a contributor to intolerance recognized in OSA management reviews from UpToDate (Kryger & Malhotra, 2022).
Sudden Physiologic Changes (Weight Gain or Loss)
Significant shifts in body weight can dramatically alter pharyngeal tissue volume and airway collapsibility. Research in Sleep (Lankford et al., 2005) shows that these physiologic changes often disrupt pressure needs, potentially provoking intolerance or causing the machine to demand higher pressure than before.
Emergence of Central Sleep Apnea
Sometimes pressure escalates because the device misinterprets irregular airflow or unstable breathing patterns as obstructive events, when they may actually be central in nature. This emergence of central apnea under PAP therapy is described in the Comprehensive Physiology Study (Javaheri & Dempsey, 2013), where the brain temporarily stops signaling the muscles to breathe.
Nasal Obstruction or Elevated Nasal Resistance
Temporary congestion, seasonal allergies, or structural blockages can significantly increase nasal resistance. When this happens, APAP machines often respond by raising pressure to overcome the blockage, a phenomenon discussed in the Journal of Clinical Sleep Medicine (Yeom et al., 2021) as a key contributor to pressure variability.
Alcohol or Sedative Use
The use of alcohol or sedatives before bed relaxes the airway muscles, increasing the likelihood of collapse during sleep. Machines detect this increased instability and respond by raising pressure to compensate, a reaction supported by pharmacologic respiratory data in the American Journal of Respiratory and Critical Care Medicine (2014).
Post-Surgery Changes
Surgeries that affect the nasal passages, sinus cavities, or oropharyngeal structures often result in inflammation that temporarily increases airway resistance. During the recovery phase, your machine may respond to this restricted airflow by prompting pressure rises that feel uncomfortable until healing is complete.
Equipment & User-Related Causes
Wrong Mask Type for the Pressure Level
Using nasal pillows or minimal contact masks at very high pressures can sometimes lead to destabilization and leaks. These leaks often provoke the machine to compensate with even more air, aligning with reports on leak-related intolerance in the Chest Journal (2007).
Mask Leaks Causing APAP Compensation
Auto-CPAP machines utilize an APAP algorithm that interprets mask leaks as insufficient ventilation. Consequently, the device responds by increasing pressure to restore the prescribed airflow, often creating a cycle of higher pressure and worsening leaks known as a mask leak loop.
Aged or Degraded Cushions
Over time, silicone cushions degrade, deform, and lose their ability to maintain a secure seal against the face. This deterioration makes the device believe that higher airflow is required to maintain therapy, leading to unnecessary pressure spikes and potential expiratory intolerance.
Poor Humidifier Configuration
Insufficient humidity can cause nasal passages to dry out and swell, which increases resistance to airflow. This reaction can trigger pressure escalation, a concept supported by humidification research in the Chest Journal (Massie et al., 1999).
Incorrect CPAP Mode (APAP vs Fixed)
The APAP mode is designed to respond dynamically to resistance, but it may deliver sudden spikes if it misreads airflow patterns or if the algorithm is outdated. Switching modes without clinical guidance or failing to utilize comfort features like EPR (Expiratory Pressure Relief) or a pressure ramp can cause significant pressure instability.
What Happens When CPAP Pressure Is Too High?
When CPAP pressure exceeds what your airway requires, it fundamentally alters your natural breathing mechanics and disrupts the stability of your therapy. Instead of simply keeping the airway open, the excess force creates resistance against exhalation and destabilizes the mask seal, leading to complications that extend far beyond simple discomfort. These effects can compromise the accuracy of your treatment data and make it significantly harder to stick with the therapy long term.
Reduced Adherence
The most immediate consequence of battling high pressure is a drop in how often you actually use the machine. The physical struggle to exhale against strong resistance creates anxiety and fragments sleep, which often leads patients to skip nights or abandon therapy entirely. Research in Sleep (Ayas et al., 2006) confirms that patients experiencing intolerance to these higher settings show significantly lower adherence rates compared to those on optimized pressures.
Increased Leak Rate and Seal Disruption
Excess airflow acts like a wedge that destabilizes your mask cushion, lifting the seal away from your skin and triggering noisy, irritating leaks. Worse yet, modern machines often misinterpret these leaks as a need for more air, creating a loop of automatic pressure compensation. As noted in the Journal of Clinical Medicine (Farré et al., 2021), this improper titration and the resulting leaks lead to severe pressure misregulation and inaccurate therapy data.
Swallowing Air (Aerophagia)
When the pressure is too strong for your upper airway to manage, the air searches for the path of least resistance and is often forced past the esophagus into the stomach. This leads to painful bloating, abdominal distension, and gas upon waking. A clinical analysis in the Chest Journal (2007) highlights that excessive pressure is a primary factor associated with moderate to severe aerophagia in OSA patients.
Mucosal Dehydration
High pressure increases the velocity of the airflow passing through your nose and throat, which rapidly strips moisture from the delicate mucosal tissues. This leads to chronic irritation, inflammation, and sore throats that make therapy difficult to tolerate. According to Massie et al. in the Chest Journal (1999), balancing pressure with adequate humidification is essential to prevent the nasal symptoms and dryness caused by this continuous positive pressure.
Potential Triggering of Central Apneas
In some sensitive individuals, prolonged exposure to high CPAP pressure can overstimulate the respiratory control center, causing the brain to temporarily pause the breathing drive. This phenomenon, known as treatment-emergent central sleep apnea, occurs secondary to pressure overshoot and is discussed in detail by Javaheri & Dempsey in the New England Journal of Medicine (2013).
False Elevation of AHI
Excessive pressure frequently causes mask leaks that create turbulence and distort the airflow data (AHI readings) your machine uses to track therapy. These unstable signals can confuse the device sensors, leading to the recording of false apneas or hypopneas. The ScienceDirect Apnea-Hypopnea Index Topic Overview explains that inaccurate airflow sensing under these leak conditions can artificially inflate residual event counts, giving you a misleading picture of your health.
Why High Pressure Disrupts Therapy: Quick Physiology Card
-
High pressure increases expiratory resistance (EPAP) → breath stacking → discomfort.
-
Rapid airflow dries the mucosa and destabilizes the upper airway seal.
-
Mask leaks trigger automatic pressure compensation → circular over-pressurization.
-
Excessive pressure can desensitize chemoreceptors, occasionally leading to central apneas.
How Do You Fix CPAP Pressure That Feels Too High?
You can often fix high-pressure issues by enabling expiratory relief settings, using a ramp feature to fall asleep, upgrading to a more stable full-face mask, or switching to an auto-adjusting machine that only raises pressure when necessary.
If your CPAP pressure feels overwhelming, you don't necessarily need to lower the setting immediately. Often, the issue is how the pressure is delivered rather than the number itself. Here are eight structured ways to improve comfort and reduce the side effects of high pressure.
1. Enable Pressure Relief Features (EPR / Flex)
Goal: Decrease exhalation load.
Expiratory Pressure Relief (EPR) or Flex technology significantly improves comfort by temporarily reducing pressure during exhalation. This subtle reduction makes breathing feel much more natural and less like you are fighting the machine, thereby reducing the risk of chest fatigue and aerophagia. Advanced devices like the ResMed AirSense 11 AutoSet feature intelligent EPR control and an integrated humidifier, making them ideal choices for users who struggle to exhale against steady airflow.
2. Use Ramp or Auto-Ramp
Goal: Ease adaptation at sleep onset.
The ramp feature is designed to ease you into therapy by starting at a low, comfortable pressure and gradually increasing it to your prescribed level over a set period, usually 20 to 45 minutes. This prevents the sensation of sudden high pressure while you are trying to fall asleep.
-
Standard Ramp: Increases pressure on a fixed timer regardless of whether you are asleep.
-
AutoRamp™: Available on the ResMed AirSense 11 AutoSet, this technology detects sleep onset and begins increasing pressure only after you fall asleep, avoiding premature discomfort.
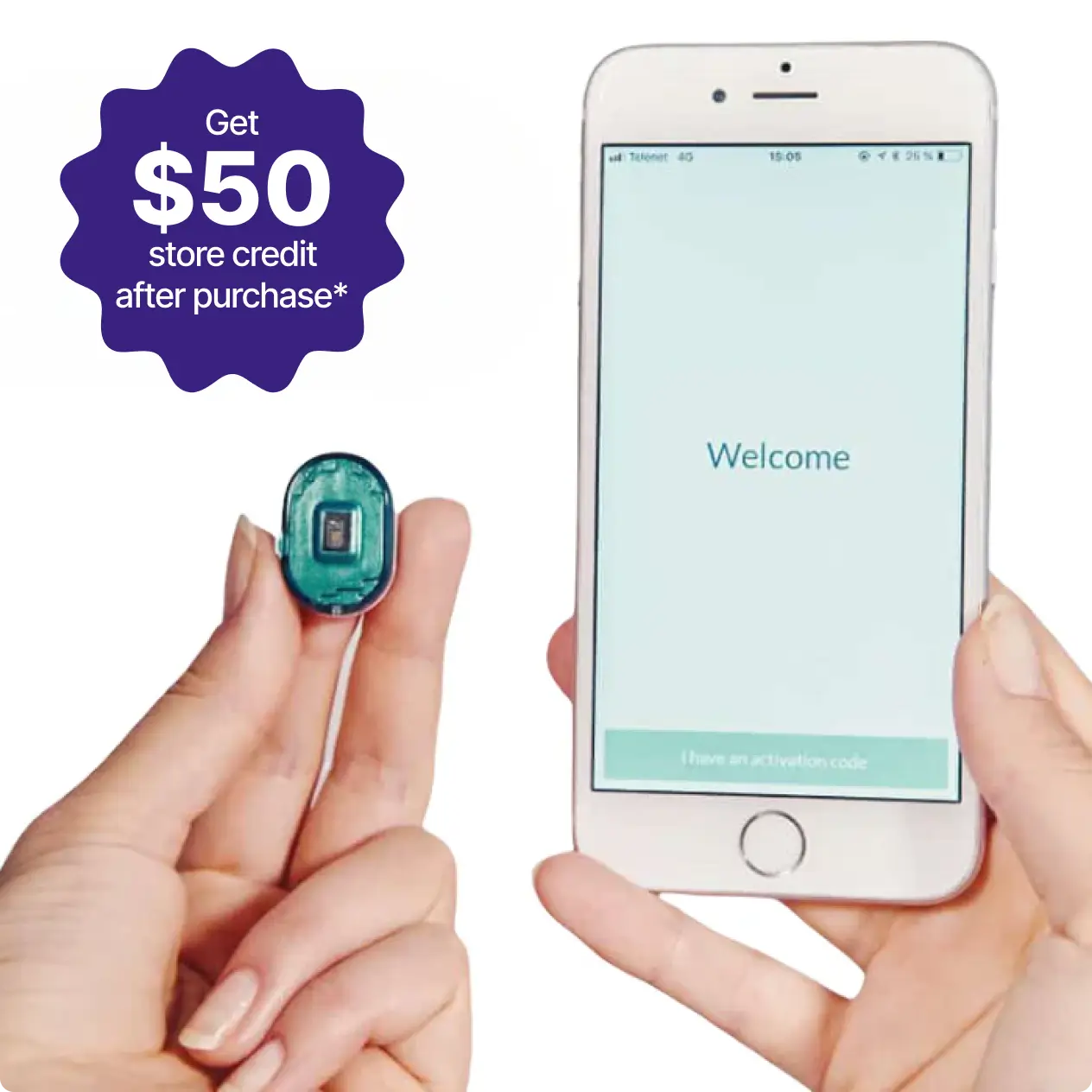
ResMed AirSense 11 AutoSet CPAP Machine Best seller Free Shipping60-Night Risk Free
Free Shipping60-Night Risk FreeResMed AirSense 11 AutoSet CPAP Machine
From$1,004.00
3. Switch to an Auto-Adjusting Machine (APAP)
Goal: Adjust pressure dynamically.
Unlike fixed-pressure CPAP machines that blast the same airflow all night, APAP (Automatic Positive Airway Pressure) machines adjust breath dynamically with each breath. They automatically raise or lower pressure in response to detected resistance or airway events, so you are only exposed to high pressure when you absolutely need it. You can explore various models in our APAP Machines collection, including the ResMed AirSense 11 Autoset, which uses an adaptive algorithm to refine nightly pressure delivery based on real-time airway behavior.
4. Upgrade to BiPAP If Needed
Goal: Provide separate inspiratory (IPAP) and expiratory (EPAP) pressures.
For some users, even EPR isn't enough to make high pressure tolerable. BiPAP machines solve this by providing two distinct pressure levels: a higher Inspiratory Positive Airway Pressure (IPAP) to keep the airway open and a significantly lower Expiratory Positive Airway Pressure (EPAP) to make breathing out easy. This split reduces intolerance significantly. The ResMed AirCurve 11 VAuto delivers customizable IPAP/EPAP support with HumidAir™ integration, while the earlier AirCurve 10 VAuto offers similar trusted performance. For those who need a broader adjustment range, the Luna G3 25A BiPAP Machine is a compact and effective bilevel option.

ResMed AirCurve 11 VAuto with HumidAir

Luna G3 25A BiPAP Machine React Health
5. Improve Mask Seal (Important for High Pressure)
Maintaining a proper seal is critical because, at higher pressures, even small leaks can trigger the machine to blow harder to compensate, creating a chaotic loop of noise and discomfort. Full-face masks are generally the most effective solution here because they distribute airflow across both the nose and mouth, making the seal much more challenging to displace under heavy pressure loads than with smaller nasal masks.
ResMed AirTouch F30i Clear Full Face CPAP Mask
The ResMed AirTouch F30i Clear combines a hybrid design and top-of-head tubing to distribute pressure while allowing even movement during sleep. Its UltraSoft™ memory foam cushion reduces facial contact and prevents red marks, a common issue at higher pressures. The foam also creates a more effective seal against heavy airflow, making it ideal for side sleepers and those who experience frequent leaks.
ResMed AirFit F30i Full Face CPAP Mask
The ResMed AirFit F30i features a lightweight silicone cushion and an open-field design for improved freedom of movement. The top-of-head hose connection helps relieve front-heavy tension and reduce tube drag, especially when high airflow pushes against the mask seal. It’s suitable for those who prefer the same structure as the AirTouch, but with a silicone alternative that’s easier to clean and longer-lasting.
ResMed AirTouch F20 Full Face CPAP Mask
The ResMed AirTouch F20 features memory-foam technology and a more traditional front-hose design. Its adaptive foam cushion conforms to facial contours, maintaining a tight seal even at high pressures. This mask works particularly well for users who experience leaks around the nose or eyes and need a full-coverage option that stays stable overnight.
ResMed AirFit F40 Full Face CPAP Mask
The ResMed AirFit F40 offers a low-profile frame and an adaptive silicone seal that flexes naturally with movement. Designed for combination sleepers, it keeps airflow consistent even when changing positions. Its compact structure minimizes bulk without compromising seal integrity, making it one of the most discreet yet pressure-resistant full face options.

ResMed AirTouch F30i Clear Full Face CPAP Mask

ResMed AirFit F30i Full Face CPAP Mask

ResMed AirTouch F20 Full Face CPAP Mask

ResMed AirFit F40 Full Face CPAP Mask
High-Pressure Mask Comparison
|
Model |
Design Highlights |
Best For |
Link |
|
ResMed AirTouch F30i Clear |
Hybrid mask with top of head tubing and UltraSoft™ memory foam cushion; reduces facial pressure marks and prevents leaks at high airflow. |
Side sleepers & users on higher pressure therapy |
|
|
ResMed AirFit F30i |
Silicone version of the F30i with a flexible cushion and top-mounted hose for easy movement and reduced drag. |
Moderate pressure users needing flexibility and less maintenance |
|
|
ResMed AirTouch F20 |
Traditional full face design with adaptive memory foam seal that maintains stability under high pressure. |
Users experiencing nasal or eye leaks at high pressure |
|
|
ResMed AirFit F40 |
Compact low-profile mask using adaptive silicone to maintain a strong seal while reducing facial bulk. |
Combination sleepers seeking minimal contact but reliable pressure control |
6. Add Mask Liners and Seal Helpers
Goal: Reinforce cushion fit and reduce skin irritation.
Sometimes a direct upgrade isn't needed, just a bit of reinforcement. Mask liners act as a soft fabric barrier that absorbs moisture and oils, preventing the micro leaks that often occur when pressure rises. Products like Snugell Full Face CPAP Mask Liners help stabilize the cushion against your skin. Additionally, Snugell Gel Nose Pads can reduce bridge pressure and skin irritation, improving overall comfort at higher pressure levels.
7. Add Humidification and Heated Tubing
Goal: Counteract dryness and prevent condensation.
High-pressure airflow can rapidly dry out your nasal passages, leading to resistance and discomfort. Using a heated humidifier counteracts this by adding essential moisture to the air. Pairing your device with heated tubing, such as the ClimateLineAir 11 Heated Tube for the AirSense 11 or the ClimateLineAir 10 Heated Tube for previous generations, ensures the air remains warm and consistent all the way to your mask. You can view options in our Humidifiers Collection.

AirSense 11 & AirCurve 11 ClimateLineAir Heated Tube

ResMed ClimateLineAir Heated Tube for Airsense 10 and Aircurve 10 CPAP Machine
8. Use CPAP Pillows to Reduce Leaks
Goal: Maintain mask seal integrity through proper head and neck position.
Standard pillows often push against the mask, breaking the seal and causing loud leaks, especially when pressure is already high. CPAP-specific pillows feature unique cut-outs that accommodate the mask and hose. The Best in Rest Memory Foam CPAP Pillow uses cooling gel and a dual-sided design to support a stable fit, while the Snugell Ergonomic CPAP Pillow offers deep side indentations to prevent seal breaks.
If these adjustments don't resolve your pressure issues, it may be time to consider a different machine type. Next, we will discuss when it is appropriate to switch to BiPAP or APAP therapy.
When CPAP Pressure Feels Too Low
CPAP pressure can feel off not only when it is too high but also when it is too low, and both states produce distinct symptom patterns that tell a different story about your therapy. While this guide focuses primarily on managing high pressure, seeing the contrast helps you identify when your airflow is insufficient rather than excessive.
High vs. Low CPAP Pressure Comparison
|
Category |
When Pressure Is Too High |
When Pressure Is Too Low |
What It Means |
|
Breathing Feel |
Hard to exhale; resistance during out-breath |
Air feels weak; may need to “pull” air in |
Mismatch between set pressure and airway needs |
|
Mask Behavior |
Frequent leaks from excess airflow |
Mask stays sealed but events persist |
High pressure displaces seal; low pressure fails to prevent events |
|
Body Sensations |
Bloating/aerophagia, chest tightness |
Snoring persists; gasping sensations |
Too high forces air; too low fails to stabilize airway |
|
Sleep Quality |
Frequent awakenings from discomfort |
Recurrent apneas/hypopneas |
High pressure fragments sleep; low pressure allows obstruction |
|
AHI Pattern |
AHI may rise due to leaks/false signals |
AHI remains high because obstructions remain untreated |
AHI instability has different mechanisms in each case |
|
Common Triggers |
Mask leak, APAP overshoot, nasal blockage |
Weight gain, nasal congestion, incorrect titration |
Each requires different clinical adjustment pathways |
As the table illustrates, an airflow mismatch manifests differently depending on the direction of the error. Low pressure typically results in insufficient airway support, meaning you might still experience persistent snoring or wake up gasping because of untreated apnea. Unlike high pressure, which feels overwhelming, low pressure leaves you with residual AHI elevation because the air is not strong enough to hold the throat open. Remember that you should never adjust these clinical settings yourself, as incorrect changes can worsen your therapy outcomes.
With all that cleared up, let’s get back into our main topic, discussing everything about high CPAP pressure. In this next section, we’ll look at the scenarios suitable for different machines.
When Should You Switch from CPAP to APAP or BiPAP?
You should consider switching to APAP or BiPAP if symptoms such as aerophagia, exhalation difficulty, or AHI instability persist despite a correct mask fit and pressure adjustments. Unlike fixed CPAP, which delivers a single constant pressure, these advanced devices dynamically adjust airflow breath-by-breath to match your changing needs. This dynamic response is often the key to solving persistent problems like chronic leaks, severe bloating, or the feeling that you are fighting against the machine to exhale.
Clinical & Physiologic Signals
1. Persistent AHI Fluctuation
If your Apnea Hypopnea Index (AHI) jumps around unpredictably or remains elevated, it often means the fixed pressure setting no longer matches your airway's needs throughout the night. As noted in the ScienceDirect AHI topic overview, static pressure may fail to address these variances, whereas auto-adjusting APAP devices respond much better to the changing severity of events.
2. Aerophagia That Does Not Improve With EPR or Lower Pressure
When painful bloating and gas persist even after lowering pressure or using expiratory relief, it is a strong sign of pressure intolerance. Switching to BiPAP is often the recommended clinical pathway because it significantly reduces exhalatory pressure, preventing air from being forced into the stomach. This aligns with findings in the Chest Journal (2007) regarding excessive pressure and with the aerophagia definitions provided by the Cleveland Clinic.
3. Inability to Exhale Against Pressure
A major reason clinicians transition patients to BiPAP is exhalation intolerance, where breathing out against the incoming air feels like hard work. BiPAP machines address this by reducing pressure significantly during the exhalation phase (EPAP), a management strategy highlighted in UpToDate (Kryger & Malhotra, 2022) for patients who struggle with standard continuous pressure.
4. Post-Surgical or Physiologic Changes
Your pressure needs are not permanent; they change with your body. Significant weight fluctuations, nasal surgeries, or other physiologic shifts can render your old fixed pressure setting obsolete. Research in Sleep (Lankford et al., 2005) emphasizes that these changes necessitate a reevaluation of therapy, often making the flexible range of an auto-adjusting machine a safer long-term choice.
5. Suspected Central Sleep Apnea Emergence
In rare cases, high fixed pressure can worsen or trigger central sleep apnea, in which the brain pauses breathing signals. As discussed in the Comprehensive Physiology Study (Javaheri & Dempsey, 2013), this phenomenon may require a switch to specialized APAP or BiPAP algorithms under strict specialist supervision to avoid over-ventilating the patient.
Equipment-Related Signals
1. Chronic Mask Leaks That Do Not Resolve With Mask Changes
When mask leaks persist, fixed-pressure machines continue blasting air at the same rate, often worsening the leak. APAP machines handle these fluctuations better by adjusting flow, though severe cases might require a mask upgrade alongside the machine switch. Full-face options like the ResMed AirTouch F30i Full Face Mask or the ResMed AirTouch F20 Full Face Mask generally tolerate higher or variable pressures better than nasal interfaces, thanks to their larger seal area.
2. Fixed CPAP Pressure Feels Too Strong Despite Ramp + EPR
If you have maximized your ramp and pressure relief settings but still feel overwhelmed by the airflow, a fixed-pressure machine may be too aggressive for you. An APAP device like the ResMed AirSense 11 AutoSet automatically lowers pressure when your airway is stable, offering dynamic support that improves comfort during transitions between wakefulness and sleep.
3. Pressure Requirements Shift During the Night
Factors like rolling onto your back, entering REM sleep, or even having a glass of wine can temporarily spike your airway resistance. A fixed CPAP cannot adapt to these moments, potentially leaving you under-treated. An APAP machine responds moment by moment, increasing pressure only during these specific events and lowering it afterward.
4. Persistent Pressure Intolerance
For patients who need high pressure to breathe but cannot tolerate it physically, BiPAP is the functional solution. By separating inhalation (IPAP) and exhalation (EPAP) pressures, devices like the ResMed AirCurve 11 VAuto or the Luna G3 25A BiPAP Machine drastically reduce the work of breathing without compromising the therapy effectiveness.
Switching Guide: Trigger & Solution Table
|
Trigger |
Why It Indicates a Switch |
Best Next Option |
Relevant Sleeplay Example |
|
Persistent AHI Fluctuation |
Fixed pressure fails to address variable obstruction events. |
APAP (Auto-Adjusting) |
|
|
Severe Aerophagia |
High continuous pressure forces air into the stomach. |
BiPAP (Bilevel) |
|
|
Exhalation Intolerance |
Patient cannot breathe out against high fixed airflow. |
BiPAP (Bilevel) |
|
|
Positional/REM Spikes |
Pressure needs change based on sleep stage or body position. |
APAP (Auto-Adjusting) |
|
|
Chronic Mask Leaks |
Fixed flow exacerbates seal breaks; requires stable pressure. |
Full Face Mask + APAP |
Note on Medical Supervision: Before purchasing a new machine or changing your therapy mode, it is essential to consult your sleep specialist. Switching from CPAP to BiPAP or APAP involves changing prescription settings that must be tailored to your specific physiology to ensure safety and effectiveness.
Symptoms That Are NOT Caused by High CPAP Pressure
It is easy to blame high pressure for every hiccup in your CPAP therapy, but often the real culprit lies elsewhere. Not every discomfort you feel comes from the airflow setting itself. Many common frustrations actually stem from mask design, sizing errors, skin sensitivities, or completely unrelated sinus issues. Understanding this distinction is vital because lowering your pressure will not fix a mask that does not fit, and it might leave your sleep apnea untreated.
-
Claustrophobia: Feeling trapped or panicked is usually a psychological response to wearing a mask, rather than a reaction to air pressure. This sensation often relates to mask coverage, with full-face models feeling more confining than minimal-contact nasal pillows or nasal masks.
-
Mask Too Tight: If you wake up with headaches, strap marks, or facial pain, it is almost certainly because you have overtightened your headgear in an attempt to get a better seal. High pressure does not cause physical pain on the bridge of your nose or forehead; that is a clear sign your mask is simply too small or pulled far too tight against your skin.
-
Allergies or Skin Reactions: Red rashes, bumps, or irritation where the cushion touches your skin are typically caused by trapped oils, harsh cleaning detergents, or a material sensitivity. The pressure of the air inside the mask has nothing to do with these dermatological reactions, which are best solved by changing your cleaning routine or trying a hypoallergenic memory foam cushion.
-
Poor Mask Fit or Wrong Mask Type: While high pressure can worsen leaks, a fundamental mismatch between the mask shape and your face will cause leaks regardless of the setting. If your mask leaks constantly at low pressures, too, the issue is poor sizing or an incompatible design, not the airflow intensity.
-
Sinus Infection or Nasal Congestion: Waking up with a stuffy nose or sinus pressure is usually due to a cold, allergies, or insufficient humidity rather than air pressure. While inflammation and congestion can make even normal pressure feel suffocating, the high pressure did not cause the infection or the blockage.
When to Seek Urgent Medical Advice
While dealing with high CPAP pressure can certainly be uncomfortable, there are specific symptoms that might indicate a more serious condition that requires prompt clinical evaluation.
-
New or Worsening Central Apnea Events: If you notice new central apneas or breathing pauses appearing in your data, this may indicate a mismatch between your pressure setting and your brain's respiratory control. This complex interaction is discussed in the Comprehensive Physiology Study (Javaheri & Dempsey, 2013), which notes that pressure must be carefully managed to avoid disrupting natural breathing signals.
-
Persistent Oxygen Desaturation: Any significant drops in oxygen saturation detected by your home oximetry devices require immediate medical attention. These desaturations often signal that your ventilation is inadequate or that other sleep-related disorders are present alongside your obstructive apnea.
-
Severe Chest Discomfort: While some muscle soreness is common, severe chest pain unrelated to normal CPAP pressure intolerance requires urgent evaluation. You must rule out potential cardiovascular causes that mimic therapy side effects but carry much higher risks.
-
Continuous or Worsening Aerophagia: Do not ignore severe or persistent aerophagia accompanied by sharp abdominal pain or significant bloating. This level of gastrointestinal distress is not a normal side effect of therapy and should be assessed by a clinician to prevent long-term complications.
FAQS
What symptoms indicate that my CPAP pressure is too high?
You will likely feel like you are fighting to breathe out against the air, or you might notice your mask blowing with frequent leaks. Other clear indicators include waking up with a dry mouth, experiencing eye irritation from escaping air, or having a bloated stomach from swallowing excess air during the night.
Can high CPAP pressure cause aerophagia or bloating?
Yes, absolutely. When air pressure is too high for your airway to handle, it forces its way past the esophagus and into your stomach rather than just your lungs. This leads to uncomfortable gas, burping, and significant abdominal bloating when you wake up in the morning.
Why does high CPAP pressure make it hard to exhale?
CPAP machines blow air into keep the airway open, but high pressure creates a heavy wall of air that you have to push against to breathe out. This resistance can cause breath stacking, chest muscle fatigue, and a feeling of suffocation if you do not use pressure relief features like EPR.
Can high CPAP pressure cause mask leaks?
Yes, excessive airflow can easily destabilize the mask cushion and lift it away from your face. This breaks the seal, causing noisy air leaks that blow into your eyes or across your cheeks, often creating a cycle where the machine blows even harder to compensate for the lost air.
Does high CPAP pressure affect AHI readings?
It can surprisingly distort your data because high pressure often causes leaks that confuse the machine sensors. This leads the device to record false events or junk data, which can artificially inflate your AHI score even if your actual sleep apnea is being treated effectively.
What causes sudden increases in CPAP pressure during the night?
If you use an APAP machine, it automatically increases pressure when it detects airway resistance, snoring, or mask leaks. Sleeping on your back, consuming alcohol before bed, or having a stuffy nose can all trigger the algorithm to spike the pressure to keep your airway open.
Can high CPAP pressure trigger central sleep apnea?
In some sensitive patients, yes. Excessive pressure can lower carbon dioxide levels too much, causing the brain to stop signaling the body to breathe briefly. This is known as Treatment-Emergent Central Sleep Apnea and usually resolves with a lower pressure setting under clinical supervision.
How do I know whether my CPAP pressure is too high or too low?
High pressure usually causes physical struggle, difficulty exhaling, and bloating, while low pressure feels weak and leaves you snoring or gasping for air. If you still feel tired or wake up choking, the pressure is likely too low, but if you fight the machine, it is likely too high.
Should I adjust my CPAP pressure by myself?
No, you should never change clinical settings without consulting your sleep specialist. Incorrect adjustments can lead to ineffective therapy, worsen your AHI, or even trigger central apnea events, so it is best to let a doctor view your data and make safe changes remotely.
When should I consider switching from CPAP to APAP or BiPAP?
You should consider a switch if you cannot tolerate the fixed pressure despite using comfort settings, or if you have severe aerophagia. APAP is better for variable pressure needs, while BiPAP is the go-to solution for patients who need high pressure but struggle significantly to exhale against it.
Why does my CPAP cause dry mouth or nasal dryness?
High-pressure airflow acts like a wind tunnel, rapidly evaporating moisture from your mouth and nose tissues. This is especially common if you have mask leaks or sleep with your mouth open, which necessitates using a heated humidifier to replace the lost moisture and reduce irritation.
Can high CPAP pressure damage my lungs or airway?
CPAP is generally safe, but extremely high pressures can cause minor lung over-expansion or chest discomfort in rare cases. However, severe lung damage is improbable, as the primary risks are usually discomfort, aerophagia, and dryness rather than structural injury.
Why does my CPAP pressure feel fine some nights but too strong on others?
Your body changes day to day based on hydration, congestion, sleep position, and fatigue levels. If you have nasal congestion one night, the same pressure might feel suffocating, or an APAP machine might ramp up higher to overcome the added resistance compared to a clear night.
What symptoms are NOT caused by high CPAP pressure?
Skin rashes, acne, and claustrophobia are typically related to the mask material, fit, or hygiene, not the air pressure. Likewise, waking up with a headache or strap marks usually means your headgear is overtightened, which is a sizing issue rather than a pressure problem.
When should I seek urgent medical evaluation while using CPAP?
You should seek immediate help if you experience severe chest pain, new central apnea events in your data, or persistent drops in oxygen saturation. These could signal underlying heart or lung issues that require attention beyond simple CPAP adjustments.
References:
-
Carley, D. W., Olopade, C., Ruigt, G. S., & Radulovacki, M. (2007). Efficacy of mirtazapine in obstructive sleep apnea syndrome. SLEEP, 30(1), 35–41. https://doi.org/10.1093/sleep/30.1.35
-
Farré, R., Gozal, D., & Montserrat, J. M. (2021). Alternative procedure to individual nasal pressure titration for sleep apnea. Journal of Clinical Medicine, 10(7), 1453. https://doi.org/10.3390/jcm10071453
-
Ibanez, G., Mercedes, B. P. D. C., Vedana, K. G. G., & Miasso, A. I. (2014). Adesão e dificuldades relacionadas ao tratamento medicamentoso em pacientes com depressão. Revista Brasileira De Enfermagem, 67(4), 556–562. https://doi.org/10.1590/0034-7167.2014670409
-
Lankford, D. A., Proctor, C. D., & Richard, R. (2005). Continuous positive airway pressure (CPAP) changes in bariatric surgery patients undergoing rapid weight loss. Obesity Surgery, 15(3), 336–341. https://doi.org/10.1381/0960892053576749
-
Massie, C. A., Hart, R. W., Peralez, K., & Richards, G. N. (1999). Effects of humidification on nasal symptoms and compliance in sleep apnea patients using continuous positive airway pressure. CHEST Journal, 116(2), 403–408. https://doi.org/10.1378/chest.116.2.403
-
Owens, R. L. (2025, April 9). Obstructive Sleep Apnea (OSA). Merck Manual Professional Edition. https://www.merckmanuals.com/professional/pulmonary-disorders/sleep-apnea/obstructive-sleep-apnea-osa
-
Turek, F. W. (2006). Musing about melatonin and sleep: It’s all about timing. SLEEP, 29(5), 606–607. https://doi.org/10.1093/sleep/29.5.606
-
UpToDate. (n.d.). UpToDate. https://www.uptodate.com/contents/obstructive-sleep-apnea-overview-of-management-in-adults
-
Volkow, N. D., & Swanson, J. M. (2013). Adult Attention Deficit–Hyperactivity Disorder. New England Journal of Medicine, 369(20), 1935–1944. https://doi.org/10.1056/nejmcp1212625
-
Yeom, S. W., Kim, M. G., Lee, E. J., Chung, S. K., Kim, D. H., Noh, S. J., Lee, M. H., Yang, Y. N., Lee, C. M., & Kim, J. S. (2021). Association between septal deviation and OSA diagnoses: a nationwide 9-year follow-up cohort study. Journal of Clinical Sleep Medicine, 17(10), 2099–2106. https://doi.org/10.5664/jcsm.9352
-
“Apnea–Hypopnea Index (AHI)” — ScienceDirect Topics, Nursing & Health Professions. https://www.sciencedirect.com/topics/nursing-and-health-professions/apnea-hypopnea-index